Modern brain and spine surgery has reached an advanced stage in terms of what can technically be achieved. However, the more critical question today is not what can be done, but rather what should be done—and what should be avoided.
The “Less Is One” approach represents a contemporary perspective that defines surgical success not by the extent of intervention, but by accurate indication, minimal tissue damage, and preservation of neurological function. This strategy has become particularly important in brain and spine surgery, where unnecessary or excessive interventions may lead to permanent morbidity. Through this approach, recovery time is shortened and patients return to daily life significantly faster.
Beyond its clinical advantages, the “Less Is One” strategy also represents a sustainable model from an economic perspective. By prioritizing minimally invasive, well-indicated surgical interventions, this approach enables shorter hospital stays, faster patient discharge, and earlier return to daily and professional life. Reduced postoperative complications, lower need for intensive care, and minimized rehabilitation periods collectively contribute to decreased healthcare costs and improved cost-effectiveness. In this context, “Less Is One” not only enhances clinical outcomes but also provides measurable financial benefits for patients, healthcare systems, and insurers by transforming surgical efficiency into economic value.
From the perspective of insurance providers and healthcare administrators, prolonged and extensive surgical procedures significantly increase hospitalization costs, resource utilization, and indirect economic losses related to delayed patient recovery. A precision-focused, well-indicated surgical approach that minimizes operative time and tissue trauma enables shorter hospital stays, faster return to daily and professional life, and more predictable cost structures. Therefore, surgical models aligned with the “Less Is One” strategy should be actively supported as they represent a clinically effective, economically efficient, and system-sustainable approach to modern healthcare delivery.
We discussed the “Less Is One” strategy in modern neurosurgery with Dr. Caner Sarıkaya, Faculty Member at the Department of Brain and Spine Surgery, Maltepe University Faculty of Medicine, Istanbul.
Lumbar Disc Herniation Surgery: Treating the Patient, Not the Image
Lumbar disc herniation is one of the most common conditions encountered in brain and spine surgery. Although advances in magnetic resonance imaging have increased diagnostic sensitivity, it is well known that not every radiological finding constitutes a surgical indication. Accurate treatment decisions require a combined evaluation of clinical findings and imaging results.

Within the framework of the Less Is One approach:
- Surgical intervention is planned only in the presence of significant neurological deficit or pain refractory to conservative treatment.
- Targeted surgical techniques are preferred instead of extensive and unnecessary decompressions.
- Preservation of normal anatomical structures is prioritized; therefore, instrumentation (screws and rods) is applied only when clearly indicated, and minimally invasive, muscle-sparing surgical techniques are favored.
This approach reduces surgery-related tissue damage, accelerates postoperative recovery, and improves long-term functional outcomes.
Cervical Disc Herniation Surgery: Neurological Safety Through Minimal Intervention
Cervical disc herniation requires a high level of surgical precision due to its proximity to the spinal cord and nerve roots. Despite advances in imaging, not every cervical disc protrusion necessitates surgical treatment. Clinical symptoms, neurological examination findings, and radiological data must be evaluated together.

According to the Less Is One strategy:
- Surgery is planned only in cases of progressive neurological deficit or symptoms resistant to conservative management.
- Unnecessary multi-level surgeries are avoided, favoring focused interventions targeting the symptomatic level.
- In suitable patients, minimally invasive anterior approaches are preferred; when more than two levels are involved, posterior approaches may be selected. In selected posterior cases, instrumentation may not be required.
This strategy minimizes surgical complications while preserving spinal cord and nerve integrity, leading to better functional outcomes.
Spinal Canal Stenosis Surgery: Effective Decompression Without Disrupting Spinal Balance
Spinal canal stenosis is a common condition, especially in elderly patients, and carries a significant risk of overtreatment. While wide laminectomies may provide short-term relief, they can result in long-term disruption of spinal biomechanics.
Within the Less Is One framework:
- Surgery is performed only in patients with clinically significant neurological symptoms.
- Limited decompression is applied exclusively at symptomatic levels.
- Posterior supporting structures are preserved whenever possible, and fusion surgery is avoided unless instability is clearly demonstrated.
- Muscle-sparing surgical techniques using approximately 1 cm skin incisions are employed.
This approach maintains spinal biomechanical integrity and improves long-term patient satisfaction.
Spine Surgery: More Clinical Judgment, Not More Instrumentation
Instrumentation techniques play an important role in modern spine surgery. However, current scientific evidence clearly demonstrates that not every spinal pathology requires stabilization.
The Less Is One approach advocates:
- Instrumentation decisions based strictly on evidence-based indications,
- Avoidance of prophylactic or habit-driven fusion surgeries,
- Emphasizing clinical judgment over technological availability in surgical decision-making.
This philosophy reduces surgical morbidity and enables patients to return to daily life more quickly and safely.
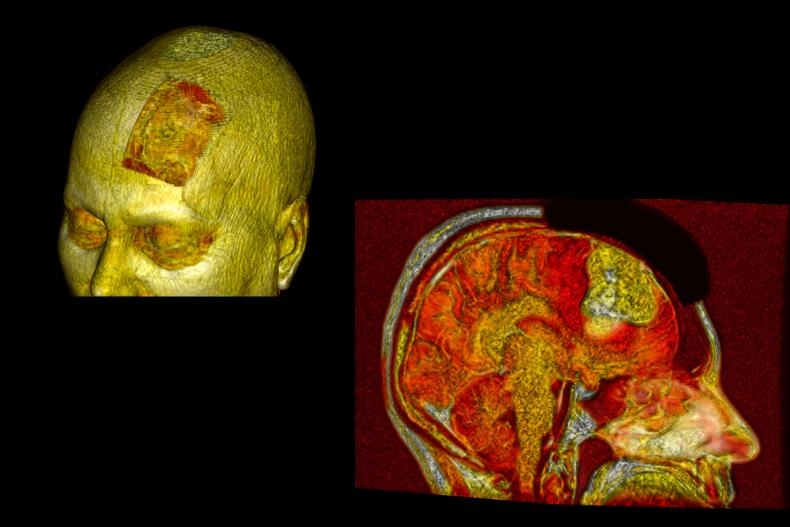
Brain Tumor Surgery: Maximal Safe Resection, Not Maximal Resection
Brain tumor surgery requires a delicate balance between oncological goals and preservation of neurological function. Although traditional approaches emphasized the extent of resection, contemporary literature highlights that functional preservation is at least as important as survival.
According to the Less Is One principle:
- The surgical objective is maximal safe resection, not maximal resection.
- Surgical planning prioritizes preservation of eloquent cortex, deep nuclei, and white matter tracts.
- In cases with a high risk of neurological deficit, subtotal resection combined with adjuvant therapies may represent a deliberate and appropriate choice.
- The use of neuronavigation and intraoperative neuromonitoring now enables maximal tumor removal with minimal damage.
This approach aims to preserve postoperative neurological function and improve patients’ quality of life.
Beyond neurological and oncological outcomes, this precision-oriented surgical strategy also yields substantial functional and economic benefits. By minimizing unnecessary tissue damage and avoiding overly aggressive resections, patients experience less postoperative functional impairment, shorter hospital stays, and reduced need for prolonged rehabilitation. Preservation of neurological function facilitates an earlier return to daily activities and professional life, thereby limiting workforce loss and productivity decline. From a healthcare system and insurance perspective, reduced hospitalization duration and lower long-term disability rates translate into significant cost savings and improved resource efficiency. Consequently, maximal safe resection not only optimizes clinical outcomes but also represents a sustainable and economically responsible model in modern brain tumor surgery.
General Approach in Brain Surgery: Surgical Precision as an Ethical Responsibility
In brain surgery, clinical decision-making is not merely technical but also an ethical responsibility. Unnecessary wide craniotomies, prolonged operative times, and excessive tissue manipulation increase morbidity without providing additional clinical benefit.
Within the Less Is One strategy:
- Targeted, minimal-access surgical approaches are preferred.
- Unnecessary exposure and brain tissue manipulation are avoided.
- Surgical decision-making considers not only what can be done, but also what should not be done.
This approach underscores that surgical mastery in modern neurosurgery is measured not by the size of the intervention, but by precision and foresight.
Spinal Fractures: Ensuring Stability While Avoiding Unnecessary Surgery
Spinal fractures may result from trauma, osteoporosis, or metastatic disease and require careful clinical evaluation. Not every vertebral fracture necessitates surgical stabilization; treatment decisions should be based on fracture type, spinal stability, and neurological status.
According to the Less Is One approach:
- Treatment decisions are guided by clinical presentation and neurological findings, not imaging alone.
- Conservative management is prioritized in stable fractures without neurological deficit.
- Surgical stabilization is reserved for cases with instability, progressive deformity, or neurological compromise.
This strategy protects patients from unnecessary major surgical procedures.
Vertebroplasty and Kyphoplasty: Effective Treatment Through Minimally Invasive Techniques
In osteoporotic vertebral fractures, pain control and early mobilization are the primary treatment goals. Vertebroplasty and kyphoplasty provide effective results when applied to appropriately selected patients.
From the Less Is One perspective:
- Vertebroplasty stabilizes the fractured vertebra through cement augmentation, providing rapid pain relief.
- Kyphoplasty aims to partially restore vertebral height and reduce kyphotic deformity.
- These procedures should be considered alternatives to extensive surgical stabilization, applied only when clearly indicated.
When used appropriately, these techniques offer shorter hospital stays, faster recovery, and earlier return to daily activities.
Not Bigger Surgery, But Smarter Intervention
In the treatment of spinal fractures and vertebral augmentation, the Less Is One approach prioritizes minimally invasive, targeted solutions over longer segment fixation, excessive instrumentation, or aggressive surgical strategies.
Success in modern spine surgery should be measured not by the magnitude of intervention, but by accurate patient selection and sound surgical judgment.
A New Definition of Surgical Success
Although modern brain and spine surgery has benefited enormously from technological advancement, true progress lies not in how much surgery can be performed, but in understanding when and how much surgery is truly necessary. The Less Is One strategy redefines surgical decision-making across a broad clinical spectrum—from lumbar and cervical disc disease to brain tumors, spinal stenosis, and vertebral fractures.
By avoiding unnecessary surgical interventions, preserving normal anatomy, and prioritizing functional outcomes, this approach enables faster recovery, earlier return to daily life, and more sustainable long-term results.
Ultimately, Less Is One is not minimalism—it is the integration of surgical maturity, clinical judgment, and ethical responsibility. In modern neurosurgery, true success lies not in larger operations, but in more precise, thoughtful, and deliberate interventions.
Economic, Social, and Workforce Impact of Precision-Based Neurosurgery
Beyond its clinical benefits, the “Less Is One” approach provides substantial economic and societal advantages across a broad spectrum of neurosurgical conditions, including spine disorders and brain tumors. By reducing operative time, avoiding unnecessary surgical extent and instrumentation, and minimizing soft tissue and neural disruption, this strategy enables shorter hospital stays, lower postoperative care and rehabilitation requirements, and faster functional recovery. Early and safe return to daily and professional life significantly reduces indirect economic losses related to workforce absenteeism, productivity decline, and long-term disability.
Conversely, patients who are unable to return to their preoperative functional and professional status following prolonged or overly aggressive surgical interventions often become dependent not only on healthcare systems but also on their families. This situation imposes a considerable caregiving, financial, and psychosocial burden on family members, leading to loss of household productivity and additional indirect costs. At a broader level, prolonged work incapacity and dependency represent an underestimated yet substantial strain on social security systems, insurance structures, and national economies. In this context, precision-driven, indication-based neurosurgical care emerges not only as a clinically sound strategy but also as a cost-effective, socially responsible, and economically sustainable model for modern healthcare delivery.
Caner Sarıkaya, MD
Department of Neurosurgery
Maltepe Üniversitesi Hastanesi
Istanbul, Turkey
E-mail: drcanersk@gmail.com
For further clinical insights and academic perspectives on modern brain and spine surgery, visit https://www.drcanersarikaya.com
Media Contact
Company Name: PR Agency: RED PRESS
Contact Person: Red Press Media
Email: Send Email
Phone: 905451552424
Country: Turkey
Website: https://redpress.net/






